Outline
Introduction
Bone strength is an essential component of skeletal health, influencing everything from posture to physical mobility and rehabilitation after injury. As research into bone biology advances, scientists have discovered that hyaluronic acid (HA)—a molecule traditionally associated with skin hydration and joint lubrication—also plays a pivotal role in maintaining and restoring bone integrity. This article explores the scientific understanding of HA’s function in bone structure, its importance in regeneration, and emerging applications that may redefine orthopedic and dental medicine.
What Is Hyaluronic Acid (HA)?
Hyaluronic acid is a naturally occurring glycosaminoglycan found in connective tissues, synovial fluid, and the extracellular matrix. It acts like a molecular sponge, holding up to 1,000 times its weight in water and creating a cushioning, hydrating effect across tissues. In bone tissue, HA is not only structural but functional—it interacts with other molecules to regulate mineralization, collagen synthesis, and mechanical stability.
HA’s Biological Role in Bone Health
Though HA is well-known for its dermatological and joint applications, its role in bone health is multifaceted. Within the bone matrix, HA contributes to:
-
Cellular communication: It facilitates the migration and differentiation of osteoblasts—the cells responsible for bone formation.
-
Nutrient transport: It acts as a medium for the diffusion of ions and metabolites, supporting mineral deposition.
-
Shock absorption: HA’s elastic nature helps mitigate mechanical stress, protecting microarchitectural bone structures.
Emerging evidence suggests HA participates directly in osteogenesis—the process through which new bone is produced—by activating cellular pathways linked to bone morphogenetic protein signaling.
How HA Contributes to Bone Strength
Bone strength is determined by both bone mineral density and its microstructure. HA influences these by improving the biomechanical properties of bone through two key mechanisms:
-
Enhancing bone density – When HA is combined with minerals like calcium hydroxyapatite, bone-forming activity increases, leading to better mineralization and hardness.
-
Improving bone matrix flexibility – HA maintains hydration and elasticity, preventing brittleness even in highly calcified tissues.
This dual role supports the balance between rigidity and resilience that defines strong, healthy bone tissue.
HA and Bone Regeneration
Recent research indicates that HA plays a vital role in bone regeneration following injury or surgery. According to a 2025 NIH study, HA enhances bone repair by promoting blood vessel development, supporting stem cell activity, and creating scaffolds for new tissue formation.pmc.ncbi.nlm.nih
In regenerative medicine, HA is often used in combination with other biomaterials such as hydrogels or 3D-printed scaffolds to mimic natural bone microenvironments. These materials provide structural support while HA accelerates cellular healing, decreases inflammation, and supports faster recovery.
The Relationship Between HA and Collagen
HA and collagen are natural partners in maintaining bone and connective tissue health. Collagen forms the framework for bone tissue, while HA provides the hydration and lubrication necessary for optimal flexibility.
A deficiency in HA can lead to:
-
Poor collagen cross-linking
-
Reduced bone elasticity
-
Increased fracture risk
Conversely, boosting HA levels through injections or supplements can improve both collagen integrity and bone microarchitecture, creating a more stable framework for bone strength and flexibility.
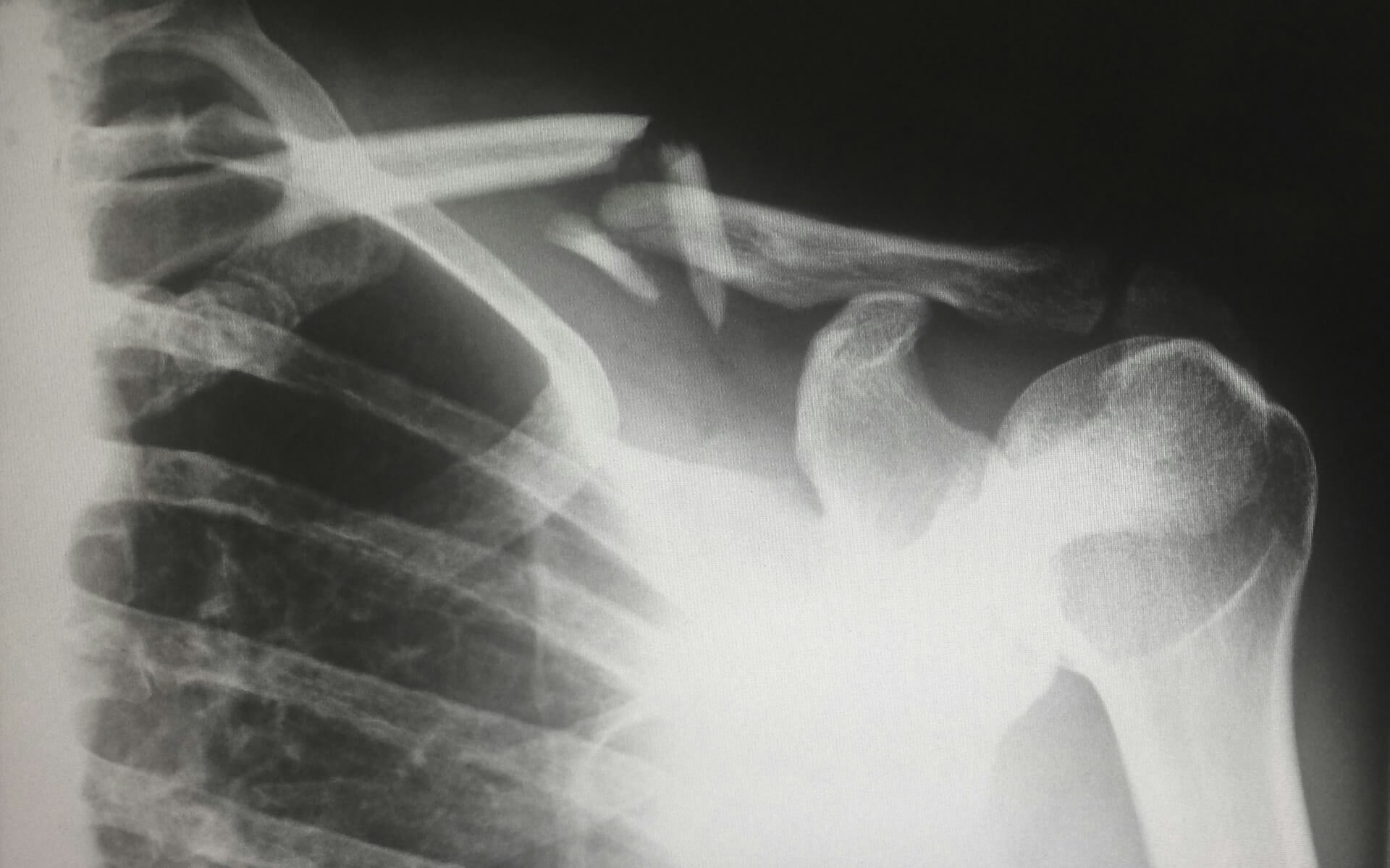
HA in Fracture Healing and Recovery
When a bone fracture occurs, healing depends on the interplay between cellular regeneration, vascularization, and extracellular matrix remodeling. Studies have demonstrated that applying HA in conjunction with bone grafts or autologous stem cells accelerates the formation of new bone tissueHA supports bone healing in three major phases:
-
Inflammation reduction: HA minimizes oxidative stress and swelling in the early healing stage.
-
Cell proliferation: It promotes the proliferation of osteoblasts and chondrocytes.
-
Bone bridging: HA stimulates the production of growth factors that connect broken bone fragments and enhance mineral deposition.
This regenerative role makes HA an appealing additive in surgical procedures involving bone grafting or orthopedic repair.
HA Supplements for Bone Health
HA supplements—often taken orally—are increasingly marketed for joint and bone health. Clinical reviews reveal they can enhance joint lubrication, alleviate osteoarthritis symptoms, and even indirectly benefit bone health by reducing inflammation.
Key supplement benefits include:
-
Improved calcium metabolism – Some formulations help the absorption and incorporation of calcium into the bone matrix.
-
Enhanced synovial protection – Maintaining healthy joint fluid reduces physical wear that can affect adjacent bone tissues.
-
Improved recovery – Oral HA accelerates reparative processes in aging adults or those with chronic musculoskeletal conditions.
Experts recommend using HA supplements alongside other bone-supporting nutrients like vitamin D and collagen peptides for a synergistic effect.
HA in Orthopedic and Dental Applications
HA’s regenerative potential extends beyond supplementation. In clinical practice, it has proven valuable in various fields:
-
Orthopedic implants: HA-based coatings improve implant integration with bone tissue, reducing rejection rates.
-
Maxillofacial surgery: HA combined with collagen promotes bone regeneration in dental implantology and sinus lift procedures, leading to stronger jawbone anchoring.
-
Cartilage repair: Joint injections containing HA not only improve lubrication but also reduce bone stress near damaged cartilage surfaces.
These applications underscore HA’s capacity to facilitate tissue compatibility and regeneration in demanding mechanical environments.
Combining HA with Other Biomaterials
One of the most promising developments in regenerative orthopedics is the use of HA in hybrid materials. Combining HA with calcium phosphate, collagen, or synthetic polymers enhances osteoconductivity—the ability of a material to support bone growth.
For example:
-
HA and calcium hydroxyapatite: Promotes superior bone bonding and biomechanical strength.
-
HA and 3D scaffolds: Improves integration in complex fractures.
-
HA and stem cells: Boosts osteoinductive activity, creating a favorable environment for bone regrowth and lubrication.
Biomedical engineers are increasingly leveraging these combinations to design grafts that mimic real bone both structurally and functionally.
Future of HA Research in Bone Regeneration
Ongoing research continues to uncover HA’s full potential in orthopedic medicine. Innovations include:
-
HA-based nanomaterials: Designed for targeted delivery of growth factors to stimulate bone formation.
-
Bioactive HA hydrogels: Engineered to match the mechanical stiffness of bone and enhance integration.
-
HA with genetic therapies: Used as carriers for DNA fragments encoding osteogenic proteins.
Despite these advancements, challenges remain—particularly in standardizing HA formulations and understanding how molecular weight variations affect its performance in bone tissue engineering. Continued exploration in both preclinical and clinical settings could eventually establish HA as a cornerstone of regenerative bone therapy.
Conclusion
Hyaluronic acid plays a far more influential role in bone health than once believed. From promoting regeneration and hydration to strengthening the structural matrix, HA serves as both a biological lubricant and a critical component of bone integrity. Whether used through supplements, medical implants, or tissue engineering applications, its integration into orthopedic science continues to expand.
The growing body of research suggests that incorporating HA—in combination with collagen, calcium, and stem-cell therapies—can significantly improve bone healing and density, especially for seniors or individuals recovering from fractures. As scientific understanding deepens, HA may redefine modern strategies for maintaining bone strength, flexibility, and long-term musculoskeletal health.